Bronchiolitis is a common respiratory condition, primarily affecting infants and young children under two years old. It is characterized by inflammation and congestion of the bronchioles, the smallest airways in the lungs, leading to breathing difficulties. While bronchiolitis is typically mild, it can sometimes progress to more severe respiratory distress and require hospitalization. Understanding the causes, symptoms, and treatment options is essential for parents and caregivers to manage this condition effectively. In this article, we will explore the nature of bronchiolitis, its causes, symptoms, risk factors, diagnosis, and effective management strategies.
Understanding Bronchiolitis:
What Is It? Bronchiolitis is a lower respiratory tract infection that inflames the bronchioles, causing them to become swollen and filled with mucus. This buildup narrows the airways and makes it tougher for infants to breathe. Unlike bronchitis, which impacts older children and adults and mostly includes the larger bronchial tubes, bronchiolitis is specific to the smallest branches of the respiratory tract.
Most cases of bronchiolitis are due to viral infections, with respiratory syncytial virus (RSV) being the main cause. Other viruses, including adenovirus, influenza, and parainfluenza, can also trigger bronchiolitis, however RSV is the predominant pathogen, especially during the winter months.
Causes and Risk Factors of Bronchiolitis
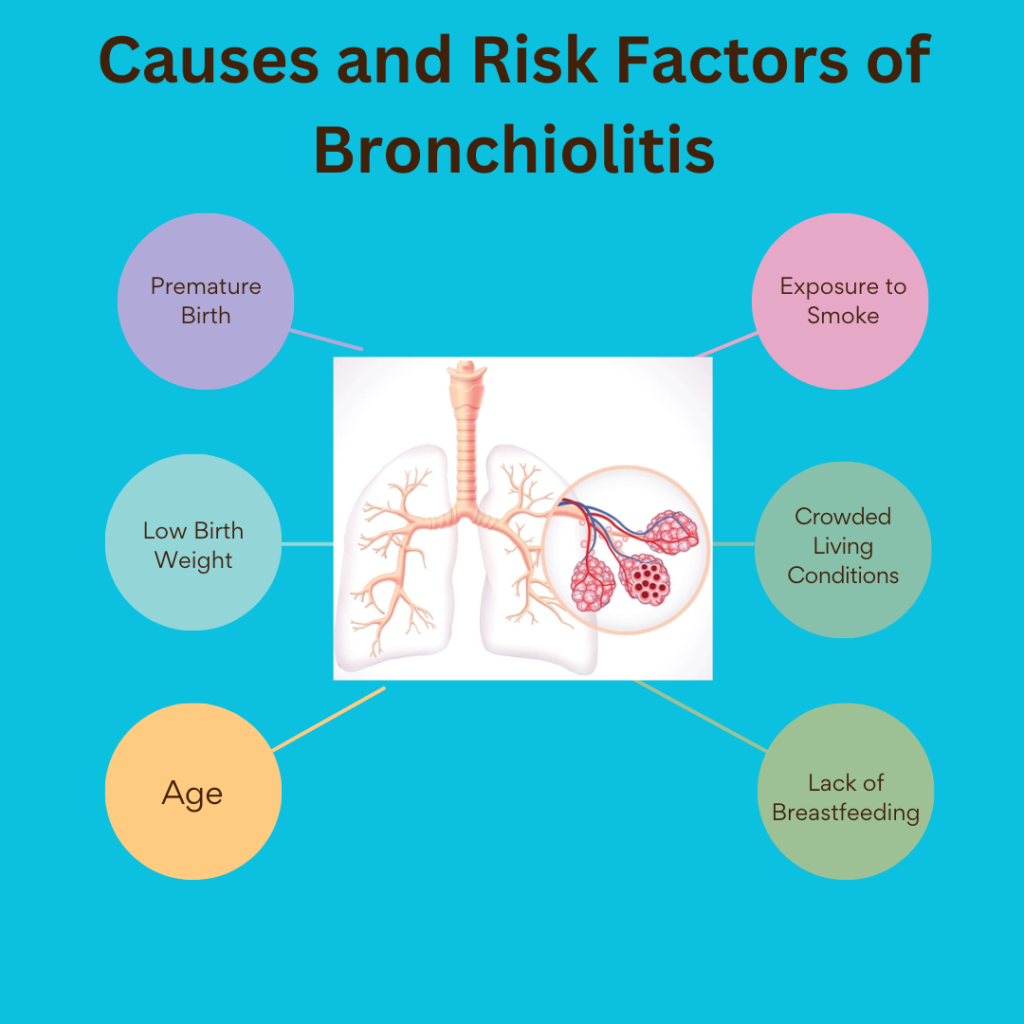
As a viral illness, bronchiolitis is highly contagious and can be easily transmitted thru respiratory droplets from coughs, sneezes, or direct touch with contaminated surfaces. The viruses causing bronchiolitis thrive in colder seasons, and cases tend to peak in the past due fall and winter months. However, numerous factors can increase a child`s risk of growing bronchiolitis or experiencing severe signs and symptoms:
- Premature Birth: Babies born prematurely have underdeveloped lungs and immune systems, making them more vulnerable to respiratory infections.
- Low Birth Weight: Infants with lower birth weights may also have much less developed respiration and immune function.
- Age: Infants below six months of age are at higher chance because of smaller airways and much less mature immune responses.
- Exposure to Smoke: Exposure to tobacco smoke or environmental pollution can irritate the airways and increase the severity of signs and symptoms.
- Crowded Living Conditions: Environments where people live in close quarters, including daycare centers, can contribute to virus transmission.
- Lack of Breastfeeding: Breastfeeding provides antibodies and immune support, so infants who aren’t breastfed can be more at risk of infections.
Symptoms of Bronchiolitis
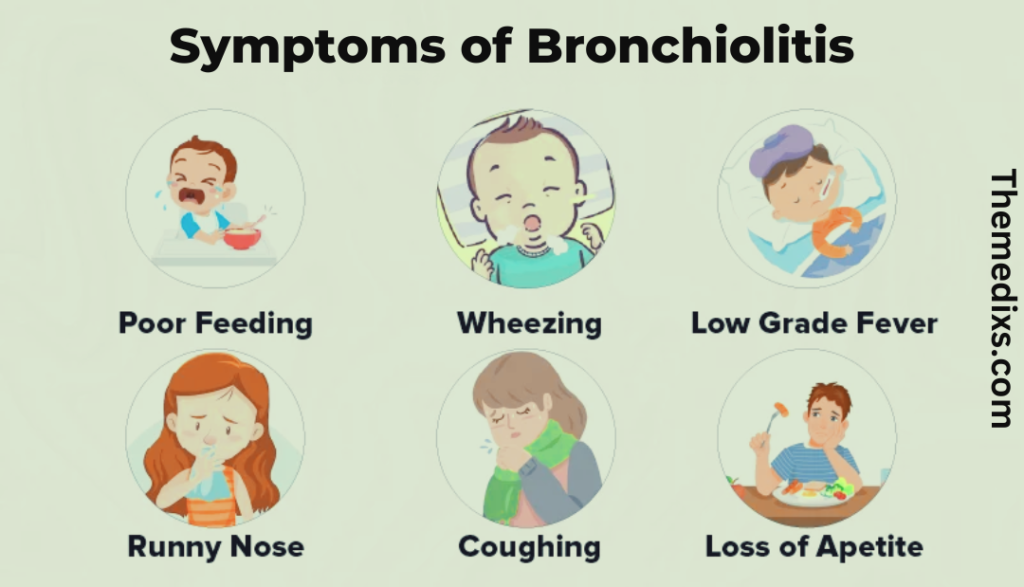
The signs and symptoms of bronchiolitis usually start with mild upper respiratory signs much like a cold, consisting of a runny nose, cough, and slight fever. However, within a few days, the signs and symptoms can progress as the infection moves into the lower respiratory tract. Key signs and symptoms include:
- Coughing: Often persistent, worsening as the airlines become more irritated.
- Wheezing: High-pitched breathing sounds, caused by the narrowing of the airways.
- Rapid, Shallow Breathing: Infants with bronchiolitis may also breathe faster and more shallowly, trying to increase oxygen intake.
- Difficulty Breathing: Some infants may also show labored breathing, with visible chest retractions where the skin between the ribs or under the ribcage pulls in with each breath.
- Flaring Nostrils: A sign of respiratory distress in infants, as they try to take in more air.
- Fatigue and Poor Feeding: Infants may struggle with feeding and become extra lethargic, as the effort to respire uses up much of their energy.
In severe cases, infants may develop cyanosis, where their lips and fingernails take on a bluish tint due to inadequate oxygen levels.
Diagnosing Bronchiolitis
Diagnosing bronchiolitis commonly includes a clinical exam by a healthcare provider. Key assessments consist of:
- Medical History and Physical Exam: The doctor will review the infant`s medical history, signs, and exposure to potential viral sources. Listening to the child`s lungs with a stethoscope helps to identify wheezing and other abnormal sounds.
- Oxygen Saturation Levels: A pulse oximeter, a small device placed on the finger or toe, can measure oxygen levels in the blood and help to determine if the child is receiving adequate oxygen.
- Chest X-rays or Lab Tests: In most cases, additional testing is unnecessary. However, if the symptoms are severe or the diagnosis is uncertain, a chest X-ray may be ordered to rule out pneumonia, or a viral test to confirm the presence of RSV or other viruses.
Managing Bronchiolitis: Treatment Options
There is no specific cure for bronchiolitis, as it is a viral illness. Instead, treatment focuses on symptom management and providing supportive care to help the child breathe more comfortably and recover from the infection. The majority of bronchiolitis cases may be managed at home, but close monitoring is essential, specifically in infants with risk factors for severe disease. Here are a few effective management strategies:
1. Hydration and Nutrition
Bronchiolitis could make feeding tough for infants because of their increased effort to breathe. Offer smaller, more common feeds to ensure they live hydrated and nourished. In severe cases, infants may require intravenous fluids in a hospital setting if they`re unable to feed properly.
2. Nasal Suctioning
Excess mucus in the nasal passages can make breathing difficult. Suctioning the nose with a bulb syringe or a nasal aspirator before feeds and naps can help clean the airway and ease respiration.
3. Humidified Air
Using a cool-mist humidifier in the child`s room can help to maintain the air moist, which can also additionally reduce airway infection and make respiration more comfortable. Be sure to clean the humidifier regularly to prevent the accumulation of mold or bacteria.
4. Oxygen Therapy
For children with low oxygen saturation, supplemental oxygen may be administered in a hospital setting to maintain ok oxygen levels in the blood. Oxygen therapy can be brought through nasal prongs or a mask, depending on the severity of the respiratory distress.
5. Medications
In maximum cases, medications aren’t necessary for bronchiolitis. Antibiotics are ineffective since the circumstance is viral, now no longer bacterial. In instances in which bronchiolitis is complicated by an underlying circumstance (inclusive of asthma), doctors may prescribe bronchodilators or corticosteroids, though these are generally not effective for routine bronchiolitis cases.
6. Hospitalization
Approximately 2-3% of infants with bronchiolitis require hospitalization, primarily because of respiratory distress or dehydration. Hospital care may consist of oxygen therapy, intravenous fluids, or close monitoring of respiration and heart rate. Infants with underlying health issues or those experiencing severe symptoms are more likely to need hospitalization.
Preventing Bronchiolitis
Preventing bronchiolitis may be challenging because of its high contagion level, however there are steps parents and caregivers can take to reduce the threat of infection:
- Hand Hygiene: Frequent handwashing is one of the most effective ways to prevent the spread of viruses. Caregivers and older siblings should wash their hands thoroughly before handling infants.
- Avoiding Crowded Places: During peak RSV season, it’s best to avoid crowded spaces like shopping malls and daycare centers, where viruses spread easily.
- Keeping Sick Individuals Away: If family members or visitors have colds or other respiratory infections, keep them away from the infant.
- Breastfeeding: Breastfeeding provides immune support and can reduce the risk of respiratory infections in infants.
- No Smoking: Exposure to smoke increases the risk of respiratory infections. Avoid smoking near infants and young children.
For high-risk infants, such as those born prematurely or with chronic lung disease, a preventive medication called palivizumab may be prescribed. Palivizumab is an injection given monthly during the RSV season to help prevent severe RSV infections.
Long-Term Outlook and Complications
Most children recover from bronchiolitis within one to two weeks, though the cough can linger for several weeks. A small percentage of children, particularly those with a family history of asthma, may experience recurring wheezing or other respiratory issues after a bronchiolitis infection. In rare cases, severe bronchiolitis can lead to complications like respiratory failure or pneumonia.
Conclusion
Bronchiolitis is a common but often manageable respiratory illness in infants and young children. By understanding its causes, symptoms, and risk factors, parents and caregivers can take proactive steps to care for children affected by the condition. While most cases can be managed at home with supportive care, it’s essential to seek medical attention if symptoms worsen or if the infant displays signs of respiratory distress. With the right care, most children make a full recovery and return to normal activities within a few weeks.