Human Immunodeficiency Virus (HIV) is one of the most significant global health issues of the past few decades. First identified in the early 1980s, HIV has since led to an epidemic that has affected millions of people worldwide. Despite extensive scientific research and advances in treatment, HIV continues to pose challenges due to its complex nature, social stigma, and the ongoing need for accessible healthcare.
This blog explores the basics of HIV, how it affects the body, its transmission, and the progress made in prevention and treatment, as well as the ongoing efforts to manage its impact.
What is HIV?
HIV is a virus that attacks the body’s immune system, specifically targeting CD4 cells (also known as T-helper cells), which play a critical role in fighting infections. Over time, if left untreated, HIV can destroy so many of these cells that the body becomes unable to defend itself against infections and diseases. This condition is known as immunodeficiency, and it can lead to acquired immunodeficiency syndrome (AIDS), the most severe phase of HIV infection.
It is crucial to understand that while HIV can lead to AIDS, not everyone with HIV will develop AIDS. Thanks to modern antiretroviral therapy (ART), many people living with HIV can manage the virus and live long, healthy lives without ever progressing to AIDS.
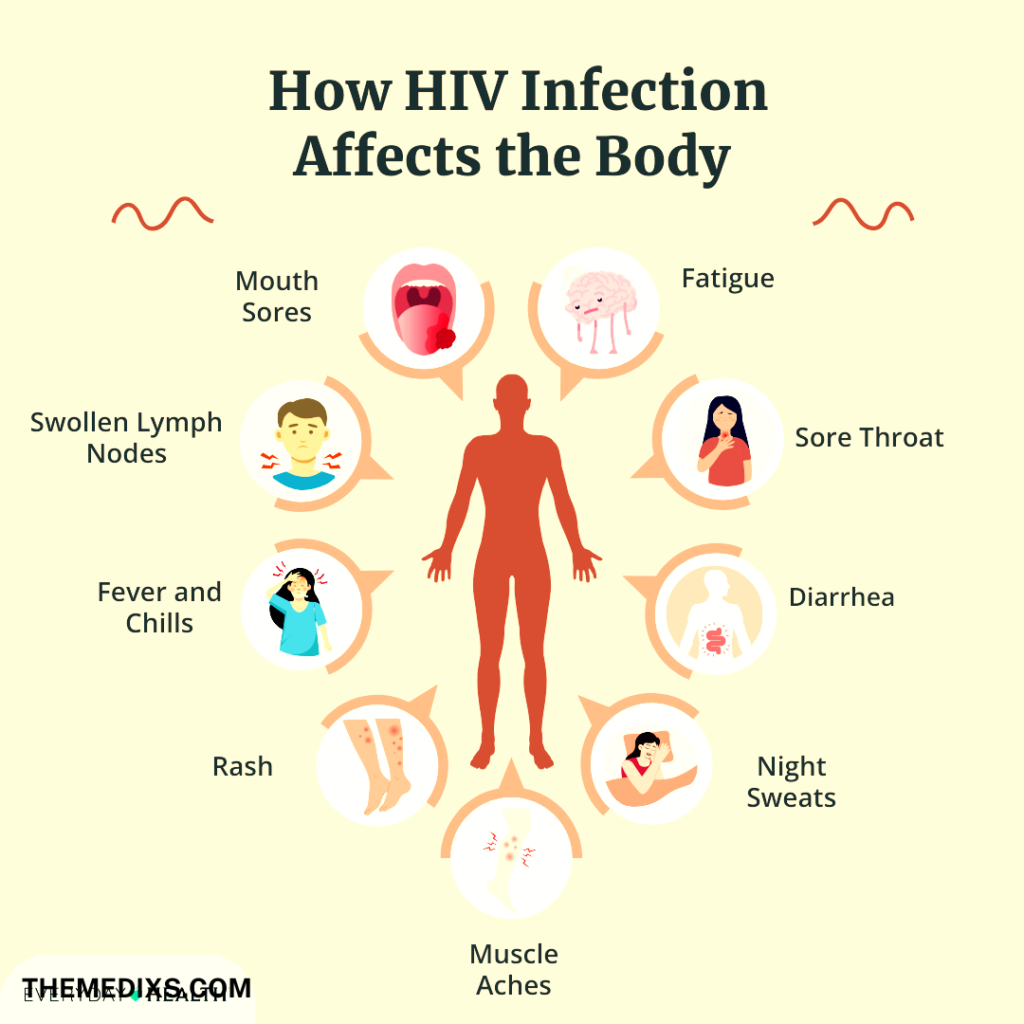
How HIV Affects the Body
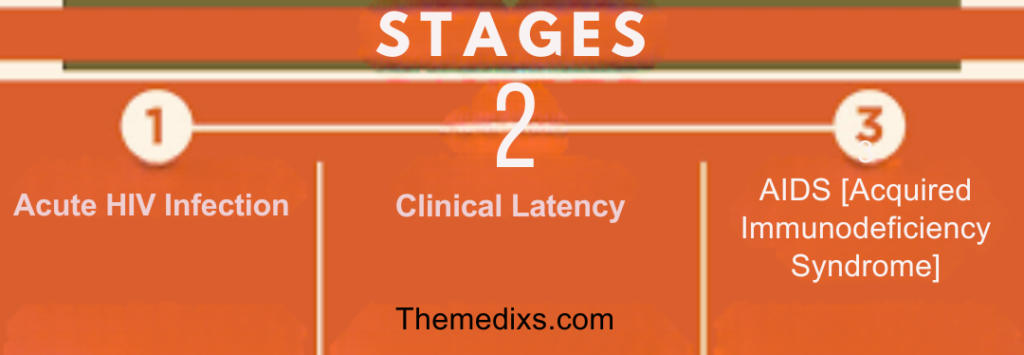
Once inside the body, HIV goes through a few critical stages:
1) Acute Infection:
Within 2 to 4 weeks after exposure, most people experience flu-like symptoms, known as acute retroviral syndrome (ARS) or primary HIV infection. This is the body`s natural response to the virus. During this phase, HIV multiplies rapidly and spreads throughout the body, with the highest concentration in the bloodstream.
2) Chronic HIV Infection (Clinical Latency):
After the initial infection phase, the virus becomes less active, though it is still present inside the body. This stage can last for numerous years, sometimes with out symptoms. However, the virus continues to reproduce at low levels, and with out treatment, the viral load will increase over time, further weakening the immune system.
3) AIDS:
Without treatment, HIV can progress to AIDS, where the immune system is severely damaged. People with AIDS are susceptible to opportunistic infections, that are illnesses that take advantage of the body`s weakened defenses. At this point, even minor infections or conditions can become life-threatening.
Transmission of HIV
HIV transmits through specific bodily fluids, including blood, semen, vaginal fluids, rectal fluids, and breast milk. It’s important to note that casual contact, such as hugging, shaking hands, or sharing food and drinks, does not transmit HIV. The primary routes of transmission include:
- Unprotected Sexual Contact: Engaging in vaginal, anal, or oral sex with out the usage of protection (e.g., condoms) can expose individuals to HIV. Anal intercourse is mainly at high-risk because of the fragile nature of rectal tissue.
- Sharing Needles: People who inject drugs and share needles or syringes are at high risk of contracting HIV. This technique of transmission is because of the direct exchange of blood, which may also include the virus.
- Mother-to-Child Transmission: An HIV-positive mother can pass the virus to her baby during pregnancy, childbirth, or breastfeeding. However, with proper treatment and care, the risk of transmission may be substantially reduced.
- Blood Transfusions or Organ Transplants: Although uncommon in countries with stringent blood screening processes, HIV can be transmitted thru contaminated blood products or organ transplants.
Myths and Misconceptions about HIV Transmission
Misinformation has historically surrounded HIV transmission, contributing to stigma and discrimination. It’s essential to clarify that HIV cannot be transmitted through:
- Casual contact (e.g., touching or shaking hands)
- Sharing food, drinks, or utensils
- Airborne transmission (e.g., coughing or sneezing)
- Using public toilets, swimming pools, or showers
Prevention of HIV Preventing
HIV transmission involves multiple strategies, which have evolved over the years with advancements in medicine and education. Some key preventive measures include:
- Condom Use: Consistent and correct use of condoms during sexual activity significantly reduces the threat of HIV transmission. Condoms act as a physical barrier, preventing the exchange of bodily fluids.
- Pre-exposure Prophylaxis (PrEP): PrEP is a daily medication for people who are at high threat of contracting HIV. When taken as prescribed, PrEP can reduce the risk of HIV transmission by up to 99%.
- Post-exposure Prophylaxis (PEP): PEP is a treatment administered within seventy two hours of potential HIV exposure. It involves taking antiretroviral medications for 28 days to reduce the probability of infection.
- Safe Needle Practices: Avoiding the sharing of needles or using sterilized equipment can prevent HIV transmission among people who inject drugs. Needle exchange programs and supervised injection sites have proven to be powerful in lowering infection rates.
- Regular Testing: Regular HIV testing is crucial, especially for people in high-danger groups. Early detection of HIV allows individuals to start treatment sooner, reducing the hazard of transmitting the virus to others and enhancing their long-term health outcomes.
- Mother-to-Child Prevention: For HIV-positive pregnant women, taking antiretroviral medications during pregnancy and childbirth, combined with avoiding breastfeeding, can dramatically lower the hazard of passing the virus to their newborns.
Treatment of HIV
Currently, no cure exists for HIV; however, antiretroviral therapy (ART) effectively controls the virus.ART involves taking a combination of HIV medicines every day. These drugs work through lowering the viral load (the amount of HIV in the blood) to undetectable levels, which helps to prevent the progression of the disease and transmission of the virus to others.
Key points about ART:
- Viral Suppression: ART can lower the viral load to undetectable levels, meaning the virus is still present in the body but at levels that can’t be detected through standard testing. People with undetectable viral loads cannot transmit HIV to others thru sex—a concept known as “Undetectable = Untransmittable” (U=U).
- Long-Term Management: For people living with HIV, adherence to ART is essential. Missing doses can lead to drug resistance, where the virus evolves and becomes more difficult to treat. Consistent use of ART helps humans maintain a healthy immune system and decrease the hazard of developing AIDS.
- Access to Treatment: One of the most important demanding situations in the global fight in opposition to HIV is ensuring access to ART, particularly in low-income countries. While significant strides have been made, hundreds of thousands of people still lack access to life-saving medications.
The Social Impact of HIV
HIV is more than just a health issue it has profound social, economic, and psychological effects on individuals and communities. Stigma and discrimination remain main barriers to HIV prevention, testing, and treatment. Many humans living with HIV face rejection, isolation, and discrimination in diverse aspects of their lives, consisting of employment, education, and healthcare.
Efforts to combat HIV-associated stigma are critical to achieving global goals of reducing new infections and improving the quality of life for the ones living with the virus. Education and awareness campaigns, along with legislation that protects the rights of humans with HIV, are vital components of the broader response to the epidemic.
The Future of HIV Research
While we have made tremendous development in the fight in opposition to HIV, the look for a cure continues. Research is ongoing in numerous areas, consisting of vaccines, gene therapy, and techniques to eliminate the virus from the body entirely. Scientists also are exploring new sorts of treatment which can require fewer doses and cause fewer side effects.
The introduction of long-acting antiretroviral drugs, administered once a month or even less frequently, promises to improve treatment adherence and enhance the quality of life for people living with HIV.
Conclusion
HIV has transformed from a death sentence in the early years of the epidemic to a manageable chronic condition today, thanks to advances in medical research and treatment. However, challenges remain, particularly in ensuring equitable access to care and addressing the social stigma associated with the virus.
By continuing to focus on prevention, early detection, and treatment, while addressing the societal issues that exacerbate the spread of HIV, we can move closer to ending the HIV epidemic and improving the lives of millions of people worldwide.









2 thoughts on “Human Immunodeficiency Virus (HIV)”