In recent years, advancements in HIV/AIDS treatment have significantly improved the quality of life for those living with the virus. However, despite these advancements, people with HIV remain at a higher risk for various types of cancer. The relationship between HIV and AIDS related cancer is complex, driven by a combination of immunosuppression, viral co-infections, lifestyle factors, and chronic inflammation. In this blog, we will explore the types of cancers most commonly associated with HIV/AIDS, discuss why these cancers develop, and highlight current strategies for prevention, detection, and treatment.
What is HIV and AIDS?
Before we dive into the topic of HIV and AIDS related cancer, it`s essential to understand HIV and AIDS. HIV (Human Immunodeficiency Virus) is a virus that attacks and weakens the immune system, making it harder for the body to fight infections and diseases. Over time, if untreated, HIV can progress to AIDS (Acquired Immunodeficiency Syndrome), the most severe phase of the infection, in which the immune system is critically damaged. People with AIDS are at a higher hazard of opportunistic infections, including certain types of cancers that aren’t as common in the general population.
Why Does HIV Increase Cancer Risk?
The increased risk of most cancers in human beings with HIV/AIDS may be attributed to numerous factors:
- Weakened Immune System: A healthy immune system can often detect and kill abnormal cells before they develop into most cancers. However, HIV weakens the immune system, making it harder for the body to fend off infections and abnormal cell growth.
- Viral Co-infections: Many cancers related to HIV are connected to co-infections with different viruses, inclusive of Human Papillomavirus (HPV), Epstein-Barr virus (EBV), and Kaposi’s Sarcoma-associated herpesvirus (KSHV). These viruses can result in most cancers, especially when the immune system is compromised.
- Chronic Inflammation: Long-term HIV infection can result in chronic inflammation, which has been related to an improved hazard of most cancers. Chronic irritation can reason cell harm and sell most cancers development.
- Lifestyle Factors: People with HIV are much more likely to engage in high-risk behaviors, inclusive of smoking and heavy alcohol use, which can increase the chance of developing certain cancers.
Types of HIV and AIDS Related Cancer
Cancers in humans living with HIV are classified into groups: AIDS-defining cancers and non-AIDS-defining cancers.
AIDS-Defining Cancers
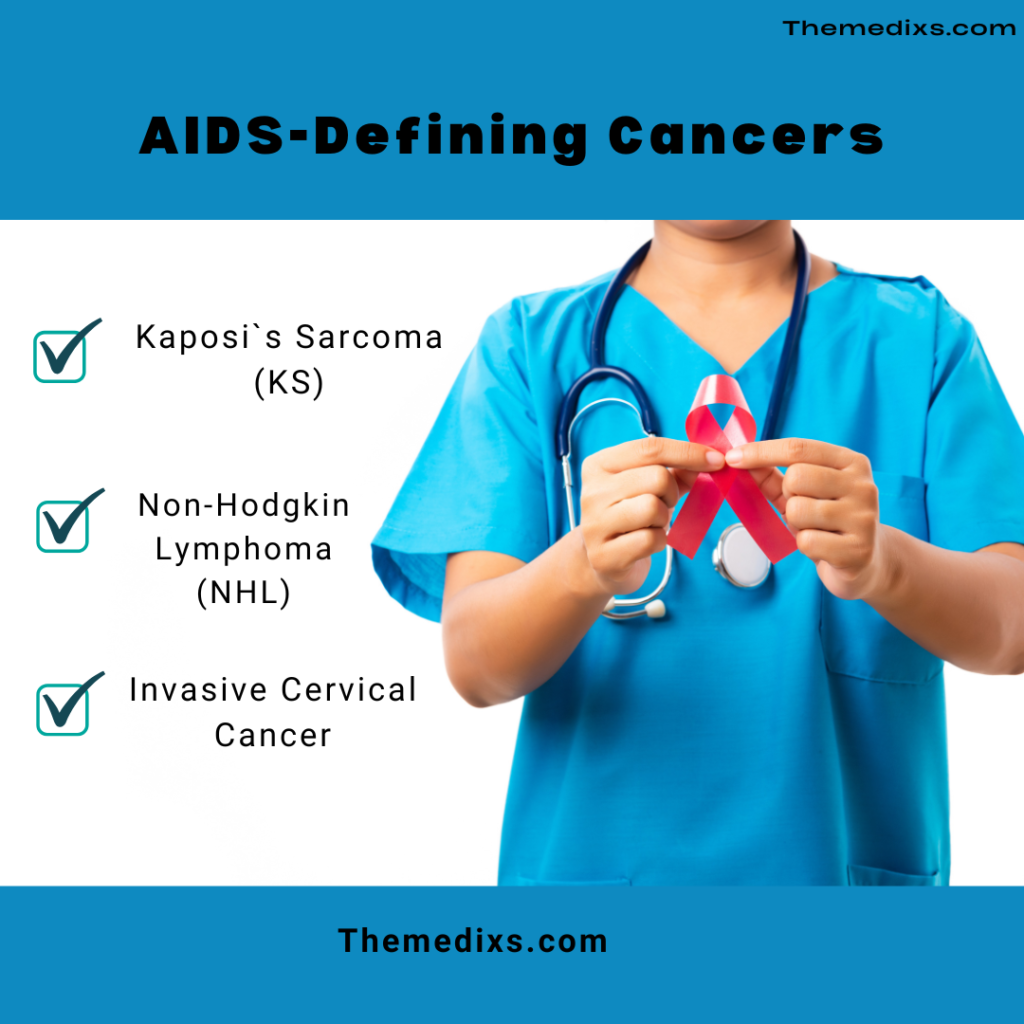
AIDS-defining cancers are cancers that are most generally related to severe immunosuppression in AIDS patients. These include:
- Kaposi`s Sarcoma (KS): Caused by the Kaposi`s Sarcoma-associated herpesvirus (KSHV), KS is a kind of cancer that affects the lining of blood and lymph vessels. It can cause purplish lesions on the skin, as well as in the mouth, lungs, and gastrointestinal tract. KS was once a common cause of death in AIDS patients but has become less prevalent with antiretroviral therapy (ART).
- Non-Hodgkin Lymphoma (NHL): NHL is a cancer of the lymphatic system and includes various subtypes. HIV-positive individuals, particularly those with low CD4 cell counts, have a significantly better risk of developing NHL, especially aggressive types like primary central nervous system lymphoma.
- Invasive Cervical Cancer: Cervical cancer is connected to infection with HPV, a deadly disease much more likely to persist in humans with weakened immune systems. Women with HIV are at a better chance of developing cervical cancers, and regular screening is critical for early detection and treatment.
Non-AIDS-Defining Cancers
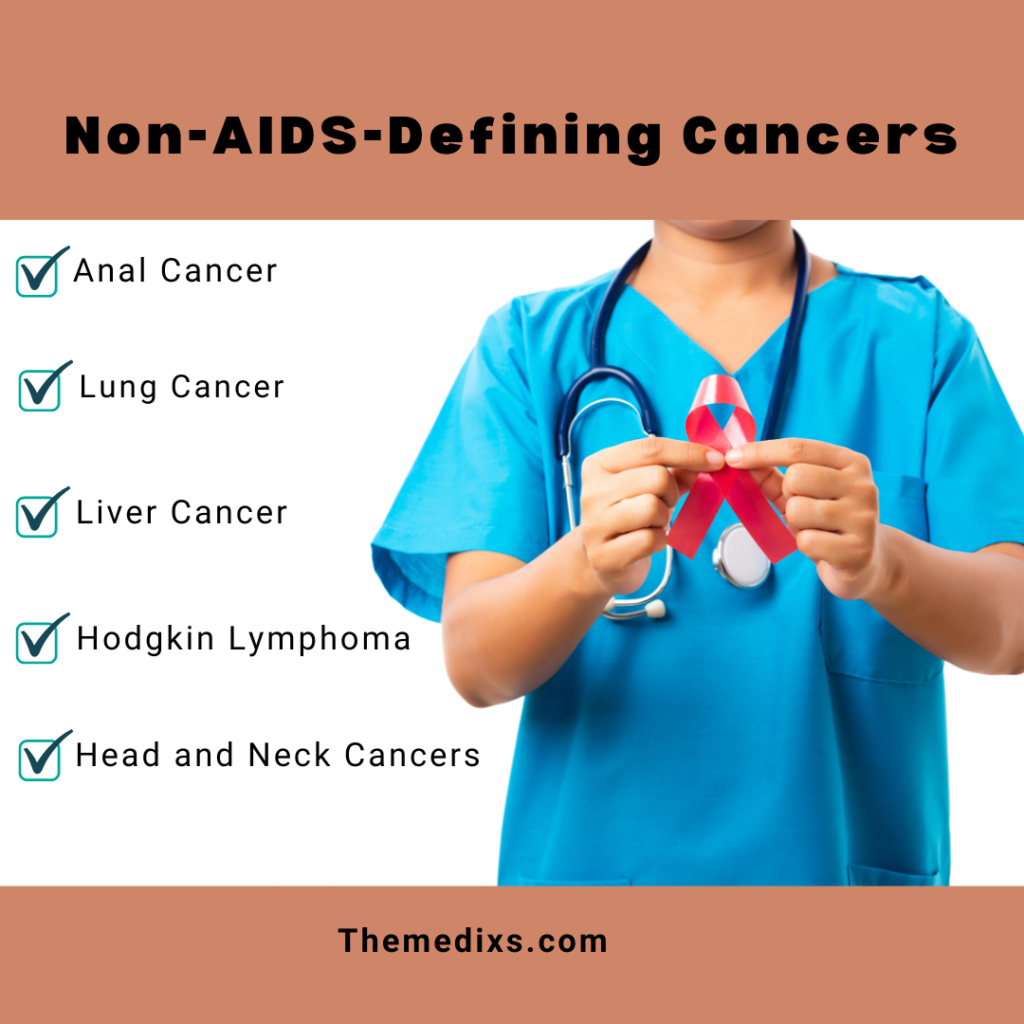
With the advent of ART, people with HIV are living longer, which has increased the risk of developing non-AIDS-defining cancers, including:
- Anal Cancer: Like cervical cancer, anal cancer is associated with HPV infection. People with HIV, especially men who’ve intercourse with men, are at a higher threat of developing anal cancer because of a combination of HPV infection and immune suppression.
- Lung Cancer: Smoking is prevalent amongst humans with HIV, which, mixed with immune suppression, will increase the threat of lung most cancers. Lung most cancers stays one of the main reasons of most cancers-associated deaths in HIV-tremendous individuals.
- Liver Cancer: Many humans with HIV additionally have hepatitis B or C virus infections, each of which might be threat elements for liver most cancers. Chronic infection from hepatitis and HIV can cause liver damage, cirrhosis, and most cancers over time.
- Hodgkin Lymphoma: Although now no longer labeled as an AIDS-defining most cancers, humans with HIV are at a better threat of growing Hodgkin lymphoma. This kind of most cancers is regularly greater competitive in HIV-tremendous individuals.
- Head and Neck Cancers: Cancers of the mouth, throat, and other areas in the head and neck are more common among HIV-positive individuals. This extended threat is in part because of HPV contamination and other life-style elements.
Prevention and Early Detection
1. Antiretroviral Therapy (ART):
ART is a cornerstone of HIV management and decreases the threat of both AIDS-defining and non-AIDS-defining cancers. By keeping HIV under control, ART helps to maintain immune function and lowers the chance of co-infections and chronic inflammation.
2. Regular Screening and Vaccination:
- HPV Vaccination: The HPV vaccine can prevent infections that lead to cervical, anal, and some head and neck cancers. This vaccine is highly recommended for HIV-positive individuals, specially young people.
- Routine Screenings: Pap smears, anal Pap tests, and colonoscopies are important screening techniques for detecting cancers early. Regular screenings for liver cancer, lung cancer, and pores and skin cancer are also recommended for humans with HIV.
3. Lifestyle Modifications:
Smoking cessation, limiting alcohol intake, keeping a healthy diet, and tasty in regular physical activity are crucial preventive steps. These modifications not only reduce most cancers threat but also enhance basic health and quality of life.
Treatment Options for HIV and AIDS Related Cancer
Treating most cancers in humans with HIV may be tough because of immune suppression, co-existing infections, and the potential for drug interactions. However, latest advances have made it viable for many humans with HIV-associated cancers to receive effective treatment. Treatment methods include:
- Optimizing and continuing ART during cancer treatment is crucial to maintain immune function and manage HIV.
- Chemotherapy and radiation therapy effectively treat many HIV-associated cancers, but clinicians must carefully control them to limit toxicity. Some chemotherapeutic agents can suppress the immune system further, so balancing effectiveness and side effects is essential.
- Immunotherapy: Immunotherapy is a more recent cancers treatment approach that harnesses the body`s immune system to combat most cancers. While immunotherapy shows promise, its effects on humans with HIV are still under study, as immunotherapies can potentially exacerbate immune system-related issues.
- Surgery: In cases where tumors are localized, surgery can be an effective option. Surgery may be combined with chemotherapy or radiation for optimal outcomes.
- Stem Cell Transplants: For aggressive lymphomas and other blood cancers, stem cell transplants have become a viable treatment option. Though complex, they can be life-saving and are increasingly successful in HIV-positive patients.
Moving Forward: Research and Hope
Research continues to explore why certain cancers are more prevalent among people with HIV and to identify potential treatments that cater to their unique needs. Ongoing studies aim to improve immunotherapy options and reduce treatment side effects for people with HIV-related cancers.
Moreover, raising awareness about cancer risks in the HIV-positive population is crucial. Education and outreach efforts can help individuals make informed decisions about their health, seek regular screenings, and adopt preventive measures.
Conclusion
The link between HIV, AIDS related cancer underscores the need for vigilance, preventive measures, and timely treatment. With early detection, lifestyle modifications, and advanced therapies, people with HIV/AIDS have a better chance of reducing their cancer risk and achieving positive outcomes if diagnosed. Collaboration among healthcare providers, patients, and researchers is essential to improve the lives of those affected and continue the progress in HIV-related cancer care.